Physical Therapy for the Mid Back
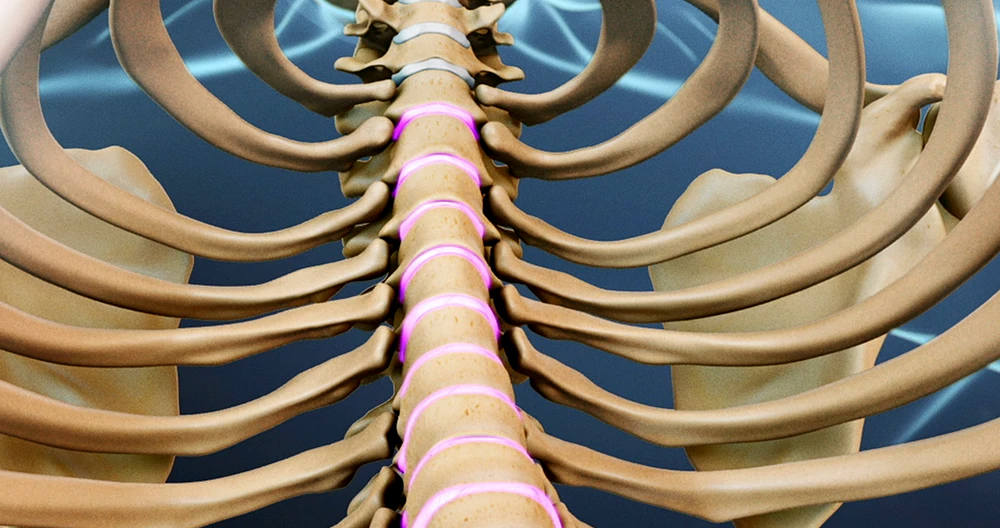
Why am I having this problem? The majority of thoracic disc herniations occur due to wear and tear. This is called degeneration. As a disc’s nucleus ages, it begins to crack and tear. These injuries can be repaired using scar tissue. As the annulus weakens over time, the nucleus may herniate through the damaged annulus. T11 and T12 are common areas for spinal degeneration. T12 is the place where the lumbar and thoracic spines meet. This link is susceptible to the forces of daily activity such as twisting and bending. It is here that most thoracic disc herniations occur.
Sometimes, however, a thoracic Disc may herniate abruptly (an acute injury). A car accident or fall can cause a thoracic disc to herniate. A sudden and powerful twist of the middle-back may cause a herniated thoracic disc.
Thoracic disc herniation can be caused by diseases of thoracic spinal nerves. Thoracic disc herniations in Scheuermann’s patients are, for example. Although evidence isn’t conclusive, it seems that patients with Scheuermann’s disease may have multiple herniated discs.
When a thoracic disc herniates, the spinal cord can be damaged. The spinal canal in the thoracic spine’s narrowest part is very dangerous. Anything that takes up space within the canal can cause injury to the spinal cord. Most disc herniations of the thoracic spinal canal push back rather than deflecting towards either side. This causes the disc material to push straight toward the spinal cord. A herniated disc could cut off the spinal cord’s blood supply. Discs that protrude into the critical zone (T4-9 of the thoracic spine) can cut off blood supply to this area of the spine. This can lead to severe paralysis and weakness in the legs.
SYMPTOMS
What does this condition feel like? Thoracic disc herniation symptoms vary. The location, size, pressing and damage to the spinal cord will all affect the symptoms.
Pain is the most common symptom. Although the pain is usually located around the injured disc, it can spread to one side or both of the mid-back. A common sensation is a band of pain around the chest. Patients might experience pins, pins, or numbness. Others report feeling weak in their arms or legs. A disc material that presses against the spine cord can also cause dysfunction in the bowel or bladder.
Disc herniations could also affect areas that are not connected to the spine. The pain from herniations of the upper thoracic spinal spine can radiate to one or both of the arms. A herniation that occurs in the middle part of the thoracic spinal spine can cause pain to radiate to the abdomen or chest, mimicking problems with the heart. A lower thoracic disc herniation may cause pain in your groin, lower limbs, and mimic kidney pain.
DIAGNOSIS
How do doctors diagnose the problem? A complete history and physical examination are necessary to diagnose the problem. Your doctor will ask about your symptoms and how it affects your daily activities. You will be asked questions such as where you feel pain and whether you feel numbness in your legs or arms. Your doctor will also ask you what activities or positions are making your symptoms worse. Next, the doctor examines your back to find out if you have any symptoms or back movements that cause pain. You are also assessed for your skin sensation, muscle strength and reflexes.
X-rays reveal the bones. Unless one or several of the discs has calcified, X-rays don’t normally show the discs. This is crucial in diagnosing thoracic disc herniation. It is quite reliable to identify disc herniation if a calcified disc appears to poke into your spinal canal on an X-ray. While it’s not known why a problem thoracic disc sometimes hardens due to calcification, past injury is one possibility.
Magnetic resonance imaging (MRI), is the best way to diagnose a herniated thoracic spine. Magnetic resonance imaging (MRI) uses magnetic waves to visualize the soft tissues. It provides a clear view of the discs, and whether any have herniated. This machine takes pictures that look like slices of an area where your doctor is interested. The test doesn’t need dye or a needle. The test revealed that many people have thoracic spine herniations, even if they don’t experience any symptoms. Doctors have suggested that thoracic spine herniations, which are not associated with symptoms, may be normal.
Doctors used myelography to diagnose thoracic Disc Herniations prior to MRI. Myelography is only half of the way to diagnose this condition. Myelography is an X Ray test. A special dye is injected in the area around the spinal canal. An X-ray will show the dye. This dye helps a doctor determine if the disc is pushing into a spinal canal.
You may order computed tomography (CT scanning). This is a detailed X Ray that allows doctors to view the body’s tissues in images that also look like slices. Images provide additional information about calcified discs. The CT scan may be combined with myelography by doctors. Myelography dye is used to highlight the spine and nerves during a CT scan. The myelography dye can be used to improve the accuracy and diagnostics of a CT scan that is used for diagnosing a herniated or bulging thoracic disc.
Thoracic disc herniations are diagnosed by doctors using MRI. When preparing for surgery to repair a herniated cervical disc, doctors may also use CT scans or myelography.
TREATMENT
What treatment options do you have?
Nonsurgical Treatment
Patients with symptoms due to a herniated thoracic disc are closely monitored by doctors, even if the herniation’s size is small. Severe neurological symptoms may develop quickly if the disc is putting pressure on the spinal chord or the blood vessels leading to the spine. Surgery is required immediately in these situations. Nonsurgical treatment is recommended unless your condition is serious or rapidly getting worse.
Your doctor may recommend immobilizing the back initially. The best way to calm inflammation and reduce pain is to keep the back still for a brief time. It might be necessary to stay in bed for a few days. This is because lying down on your back can cause pressure to nerves and discs. Doctors recommend against bed rest. They prefer that patients engage in normal activities. Patients can use pain to assess how much is too much. You can also immobilize your back with a brace for as long as one week.
Patients with thoracic disc herniation may be prescribed certain medications by their doctors. Aspirin and ibuprofen may be prescribed for patients with thoracic disc herniation. For back spasms, muscle relaxants might be prescribed. Sometimes, oral steroids are used in tapering doses to treat pain that spreads to the arms or legs.
Most likely, your doctor will have a Physical Therapist oversee your rehabilitation program. Physical Therapy focuses on pain relief, improving back movement and encouraging healthy posture. A Physical Therapist can help you develop a rehabilitation plan that will address your current condition and help prevent future problems.
Most people suffering from a herniated cervical disc can heal themselves without having to undergo surgery. Patients are usually advised to try nonoperative treatment for at least six weeks before they consider surgery.
SURGERY
Surgery may be recommended by a surgeon if patients are not improving with nonsurgical treatments or if their condition is getting worse. If the herniated disc is affecting your spinal cord, it may be necessary to have surgery. Surgeons will look for signs such as weakness in the arm or leg muscles, pain which doesn’t go away, and problems with your bladder or bowel.
This condition requires surgical treatment
- costotransversectomy or discectomy
- transthoracic decompression
- Video-assisted thoracoscopy Surgery (VATS).
- Fusion
Costotransversectomy
To open the space between the bones and the disc, surgeons use costotransversectomy. The surgeon works from the back of a spine by removing a small section of two or three ribs connecting to the spine. (Costo means rib.) The transverse process (the bony knob) on the side is then removed. Ectomy simply means to remove. This creates space for the surgeon. Small instruments are used to remove the damaged disc. Surgeons take great care to not injure the spinal cord.
Transthoracic Decompression
Transthoracic refers to the surgical approach. Trans is transliterated to mean across or through. The chest is known as the thoracic region. In transthoracic surgery, the surgeon works through the chest cavity to reach the injured disc. This gives the surgeon a clear view into the disc.
The surgeon places the patient on one side and cuts a small hole through the ribs of the thorax (the chest) on the other. The opening is then opened and instruments are placed through it. This releases pressure from the spinal cord (decompression).
Video-Assisted Thoracoscopy Surgery
VATS (video assisted thoracoscopy) is one of the latest developments in thoracic surgical. The procedure uses a thoracoscope (a tiny television camera) that is inserted into the side-of-the-thorax via a small incision. The surgeon can view the area in which he or she is working with the camera. Other instruments can be used during the procedure by making small incisions. While repairing and cutting damaged disc portions, the surgeon can see the TV screen.
Cutting and removing damaged parts
As minimally invasive surgery (VATS), it is less taxing on patients. Advocates claim that this type is less invasive, reduces scarring around nerves and joints, and speeds up recovery.
Fusion
The disc may be removed in part or whole. This can cause the spine to become loose and unstable. Following surgery, fusion may be required. Arthrodesis, which is the medical name for fusion, can be described as a procedure that involves locking the vertebrae in place. This procedure stops movement between the vertebrae and locks them in their place. This helps to stabilize the bones and relieves pain. Fusion surgery is rarely necessary if there was only a small amount removed from the bone and disc material during surgery to fix a herniated or bulging thoracic disc.
This procedure involves placing small grafts (or a combination of them) of bone over or under the loose spinal bones. The surgeon may use a combination cable, rods, and screws to stop the vertebrae from moving while allowing the graft to heal.
REHABILITATION
What should I expect during my recovery?
Non-surgical Rehabilitation
Even if you do not need surgery, your doctor may recommend you consult a physical therapist. Patients usually see their Physical Therapist once a week for between four and six weeks. The goals of treatment include controlling symptoms, finding positions that relieve pain, and teaching you how to keep your spine healthy during everyday activities. Patients can progress to a series of strengthening exercises as their bodies heal. Aerobic exercises such as swimming or walking can help ease pain and improve endurance.
After Surgery
Recovery after surgery can be complicated. Some patients have to leave the hospital soon after their surgery. Some surgeries require that patients remain in the hospital for a minimum of a few days. Patients who have to stay in hospital for a while may be seen by a Physical Therapist shortly after their surgery. The sessions are designed to help patients move more easily and avoid putting additional strain on their backs.
Patients are advised to follow the surgeon’s advice regarding wearing a brace or support belt during recovery. In the first few weeks following surgery, patients should be careful not to overdo activities.
Many patients who have had surgery need Physical Therapy outside of the hospital. The type of surgery may require them to see a Physical Therapist for a period of one to three years. Physical Therapists can use heat, ice or electrical stimulation to treat pain and muscle spasm. The Physical Therapists then show patients how to move safely and with the least strain for the healing process.
As patients heal, they can gradually take up flexibility exercises for the shoulders and hips, as well as mobility and strengthening exercises for the back muscles. Patients can also meet with the Physical Therapist at a swimming pool. Patients will be able to perform exercises that increase endurance, muscle strength, or alignment of the body. As rehabilitation programs evolve, patients are required to perform more challenging exercises. Safely increasing strength and functionality is the goal. In the ideal scenario, patients can return to their old activities. To avoid future problems, patients might have to alter their activities.
Once treatment is complete, regular visits to a Physical Therapist’s office will be discontinued. Although the Physical Therapist will remain available to help, patients will take responsibility for their exercise routines as part of their ongoing home program.