Intervertebral Discs are found between the vertebrae of the spine. They act as shock absorbers. Two components are found in discs and they can often be compared with jelly donuts. The annulus is the outer part of a disc. It’s made of fibrous tissue, similar to a tire. The nucleus is located in the middle of the disc. The nucleus contains protein molecules which attract fluid, which acts as a cushion and shock absorber between vertebrae.
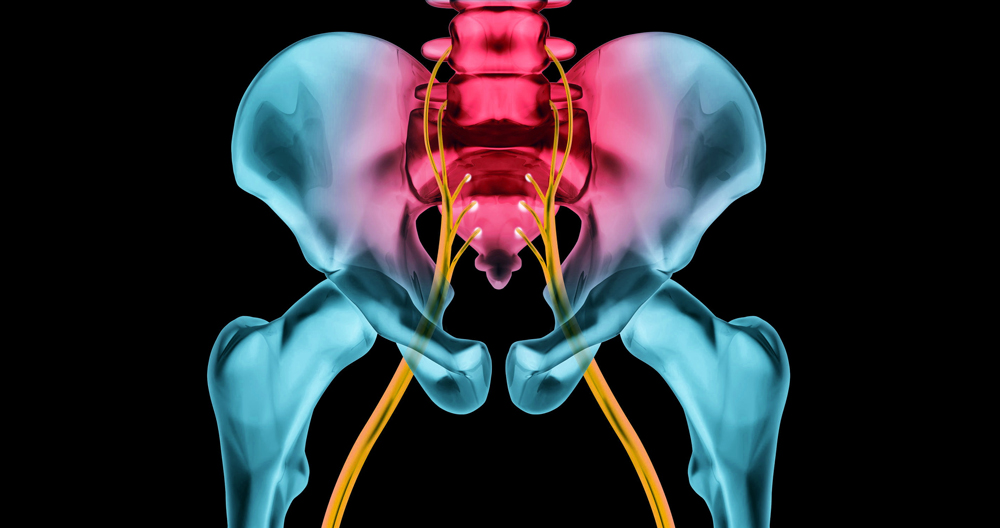
Disc herniation occurs when nucleus material located in the center of the disc is displaced through a tear, crack or rupture in the outer annulus. The most common defect in the annulus lies at the back. When this happens, the nucleus material spills into the spinal cavity. It can cause sciatica (leg pain) or irritation to a nerve root. Sciatica, which is a very severe form of leg pain, can be caused by a defect in the annulus. Sciatica is often described as worse than childbirth and kidney stones. Most people with disc herniations experience sudden, severe leg pain. A disc herniation can be caused by any injury or incident. It can happen in all walks of life and affects everyone. It’s most common for people between 20-50 years old. The disc tear may cause some people to experience some back pain.
The degree of leg pain will depend on the type of disc that has been herniated. This will determine which nerve root is affected. The 2nd and 3rd lumbar vertebrae, respectively (L4-5 and L5S), are the most common places disc herniations occur. Both can lead to pain that runs from your buttocks to your foot or calf. Some people feel numbness in the foot or leg. Sometimes they also experience weakness in the leg. However, 80 to 90% of people will recover without any special treatment. Most people recover within three to four months. Ten to twenty percent don’t fully recover.
Sometimes, pain relief can be achieved through physiotherapy and chiropractic manipulation. The majority of people will experience a gradual improvement in the symptoms of disc herniation, regardless of which treatment they receive. This is the normal history. Some disc herniations disappear completely, while for others, the pain doesn’t. The release of an inflammatory chemical that works to both dissolve the disc, and also to irritate nerves has been suggested by studies. The pain will go away once this inflammation process has ended. The nerve can be compressed by stretching the legs, which can irritate it and cause more pain. It is important that you remain active but do not cause further pain. You can avoid aggravating your pain by doing things such as pool therapy, walking, and cycling. You have a low chance of nerve damage if you remain active. Nerve injury occurs in less than 10% of disc herniations. The most common time nerve damage occurs is when the pain starts. It is very rare for nerve injury to occur later.
A herniated disc can be removed to relieve pressure on the nerve. This will provide almost instant relief for the leg pain in around eighty-nine percent to ninety per cent of people. There are some risks involved in surgery like nerve injury or infection. Surgery is generally the last resort. In less than 1 percent of cases, complications may occur. One hundred people will suffer some form of permanent nerve damage as a result of disc herniation. This can cause permanent pain, weakness and numbness.
Sciatica sufferers are often scared to return to normal activities due to the intense pain. About 10% of patients who experience recurrent disc injuries after their symptoms improve are at risk. Recurrence can happen whether the patient had surgery or not. It can occur quickly or over time. Most people can fully recover from a disc rupture and return to their full activities, such as work and leisure. Regular exercise to strengthen your core is an effective way to avoid disc herniation in the future or back pain.
Sciatica vs Herniated Disc
Doctors have been faced with new challenges by the internet. The most grave problem is self-diagnosis. The internet has a huge amount of information. It is possible to find information about anything, from Ancient Rome to Elon Musk’s newest business venture. It doesn’t necessarily mean all information on this thing-as-ma-jig will be correct.
However, this doesn’t mean that you don’t have a personal diagnosis, even though the information you find may be accurate. You are not a medical professional, and most of you aren’t either. These diagnoses are made by doctors and therapists who use sophisticated diagnostic tools. These tools cannot be found on the internet so you won’t be able to diagnose yourself using WebMD.
I wanted that out before I answered the question, “What is the difference between sciatica and herniated disc?” I’ve had patients swear up and down that they had either sciatica or herniated disc based on what they had read online. There are subtle differences in the sciatica vs. herniated-disc debate.
When I have had to tell them my diagnosis was “off”, they have given me everything, from blank stares to tears. The two conditions can be related, but sciatica is not the same thing as a herniated spine. Let’s examine sciatica vs herniated disc.
Sciatica
The sciatic nerve, which is the longest in your body, is the largest. The sciatic nerve is located in the spine. It is made up of 5 nerve roots. Dysfunction in this nerve can lead to burning, tingling and pain while sitting or walking. It can be as severe as pain as far as the feet.
Herniated Disc
These cushion-like parts, which look similar to a sponge, are filled with a fluid-like gel that protects your vertebrae. This fluid can be pressed against the disc’s hard outer shell to cause herniation. It causes pressure on the nerves which leads to pain.
The difference
Sciatica is a condition that can be treated in a very short time. For herniated spines, care is required. These discs can be a life-threatening condition. These conditions can cause severe impairments to your quality of living.
It is easy to mistake the two conditions for one another at the outset. It can be difficult to identify which condition is active without the diagnostic tools discussed earlier. Sometimes an MRI is needed to confirm a diagnosis. While a herniated or bulging disc can occasionally cause sciatica, the reverse is rarely true. These are the most important differences between sciatica, and herniated disc.
Selective Nerve Root Blocks
What are selective nerve-root blocks? A selective nerve root block is a spinal procedure where anesthetics are applied to specific nerve roots of the spine. This helps identify the exact cause of leg discomfort. This procedure can be used to diagnose the problem and determine the most appropriate level of surgical intervention or injection. Injections are often accompanied by steroid injections to lower inflammation and pain. The injection is similar in function to a transforaminal Epidural Steroid Injection, however the medication is not allowed to enter the epidural area. The aim is to simply cover the nerve root.
What is the procedure for epidural injections of steroid and selective nerve root blocks?
The fluoroscopic radiograph is typically taken with the patient lying on its stomach. Before the injection is done, you must thoroughly wash your skin with antiseptic solutions. After the skin has been anesthetized with local anesthetic, the needle is placed under fluoroscopic guidance in the proper position of the spine.
For epidural steroid injections, and for selective nerve root blocking, the needle should be just above the target root. A caudal approach is used to inject epidural steroids. The needle is passed through an opening (sacral artery) located just above the tailbone. The interlaminar approach to epidural injections involves passing the needle between two vertebrae. This is usually done at the midline. To verify the position of the needle, a contrast dye can be injected.
The medication is then given. The procedure takes approximately 15 to 30 minutes and involves close monitoring of vital signs. After the procedure, the patient will be taken to the postprocedure area where they will continue monitoring.
What exactly is injected?
Injections are usually composed of a mixture between a local (e.g. Marcaine (r), Lidocaine), and a steroid (e.g. Dexamethasone/Celestone).
Is the procedure painful or not? Not often. Most patients agree that it is no more painful than a routine blood test.
What should I expect when the procedure is over?
Anesthetic may cause temporary numbness around the nerve root or epidural spaces. The steroid medication might begin working within 6 to 3 hours after the injection. Some people feel soreness from the injection for as long as two days. You can try applying ice to help with this discomfort. You might notice significant pain relief in as little as one to five business days.
What should you do after the procedure?
After the procedure you will need someone to drive you home. It is recommended that patients restrain their activities for a few days after the procedure. Apply ice to the injection site if there is any discomfort.
How soon can you return to work?
You can go about your normal life as soon as the procedure is over.
What is the recommended number of shots that I get?
We usually do not inject more than three times in 12 months. Side effects of the steroid may occur if you receive too many injections.
Are there any possible risks involved in this procedure?
This procedure is considered very safe. Like any procedure, there can be side effects or complications.
The side effects of epidural injections and selective nerve root blocking include:
- Common: Pain at the injection site
- Sometimes there is a worsening of symptoms
- Infection – rare
- Bleeding – rare
- Extremely rare: Serious nerve and spinal cord injuries
Other side effects can be caused by steroid medications and include:
- Fluid retention – uncommon
- Weight gain isn’t common
- Elevated blood pressure – not uncommon
- Rare mood swings
- Insomnia is rare
Suppression of cortisone’s natural production by the body – rare
Is it possible to have this procedure even if you are on Coumadin® or any other blood thinners
No. No. The doctor may ask that you temporarily stop taking blood-thinning drugs.
Who should not receive an epidural injection of steroid or a selective root block?
If:
- If you have bleeding issues or are taking anticoagulant medication (blood thinner), it is possible to be at increased risk.
- Back pain can be caused by an infection or malignancy.
- Local skin infections or systemic bacteria infection are not likely to be present at the injection site.