Nonsurgical treatments are used to treat conditions affecting the L5–S1 spinal motion segment. Surgery may be necessary if the symptoms of lower back or leg pain persist or worsen despite all other treatments.
What is L5-S1 Fusion Surgery?
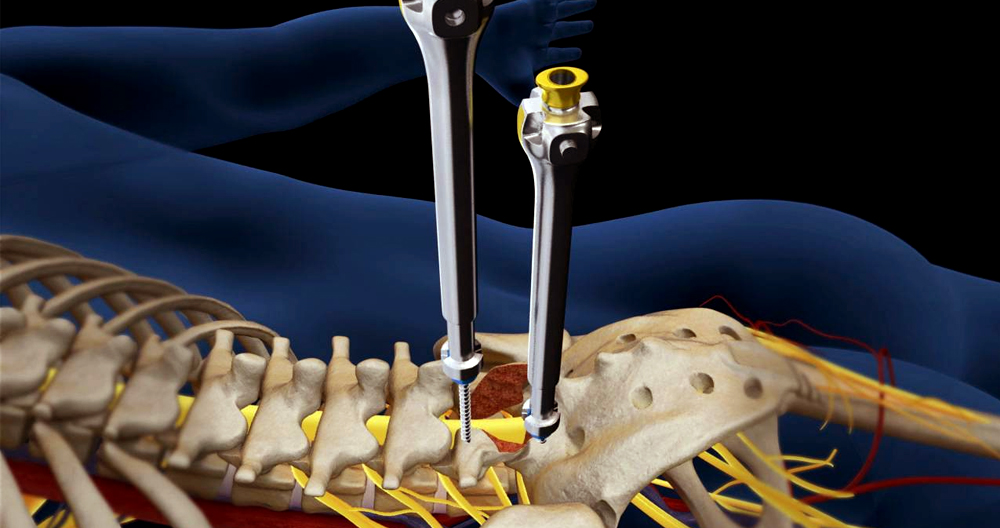
Spinal Fusion is a major procedure that involves the joining of one or more vertebrae (or spinal bones) using bolts, screws, or plates. The hardware can be placed at the front (anterior), or back (posterior). Sometimes, the disc between the spine bones is removed and replaced by bone or a spacer. The level of surgery is called L5 S1 Fusion.
The low back contains 5 spinal bones, which are numbered L1, L2, and L3, as well as L4, L4, L5, L4, L5, and L5. A disc is found between the spinal bones. The two spinal bones that it is sandwiched between are the disc’s names. The L5/S1 disc is the lowest disc in the lower back. The L5/S1 disc is located between the L5/S1 and S1 spinal bone. L5 S1 Fusion Surgery involves the surgical removal and fuse of the L5/S1 disc with the L5/S1 spinal bones. There are many surgical approaches and techniques. The case of posterior lumbar interbody Fusion (PLIF) has been discussed in detail in an earlier blog.
What are the Signs of L5 S1 Fusion?
Lumbar fusion has become a very popular procedure. The number of lumbar-fusion surgeries in the United States has increased from 77 682 to 210 407. Lumbar fusion is a treatment for a variety of degenerative and painful conditions. L5 S1 Fusion is most commonly used to treat low back disc degeneration.
What is Spinal Fusion Major Surgery?
Absolutely! To access the disc, you will need to cut through important muscles, ligaments and tendons. After the disc is removed, the area is filled with bone and sometimes a spacer. Screws are then placed in the spinal bones, above and below the disc. Additional hardware, such as plates or rods, is used to stabilize the screws.
What is the success rate of spinal fusion surgery?
It is hard to measure success in spinal fusion surgery. Why? There are many variables to consider, including the surgical approach, preoperative MRI and x-ray findings, results from pressing the disc, patient age, medical history and the parameters being studied.
The following is an example of the results: 53 patients were followed up for 20 months on average after fusion surgery. Only 50% of patients who had normal MRIs before surgery were able to see improvements after the procedure.
40 percent of patients who had lumbar fusion 2 years ago were unsatisfied or unsure about the results, reporting continuing back pain and limited daily functioning. Another study found that the failure rate for lumbar spine surgery is between 10% and 46%. These statistics would show that l5 and s1 surgeries are successful rates.
Spinal Fusion: Can Screws Be Removed?
Yes! Yes! Failure to fuse the bones properly is the most common type of fusion.
Non-Union
Non-union is when spinal bones that have been bolted together fail or do not fuse together. The rate of non-union will vary depending on the type of lumbar spine fusion. Non-union rates can reach as high as 23 to 36 percent for procedures that involve more bone, such as posterior fusion.
Broken Screws in Lumbar Fusion
Lumbar fusion is a procedure that involves the use of screws, bolts, plates, and other devices to stabilize the spinal bones. The hardware and low back are subject to significant forces. Unfortunately, these forces can cause spinal instability and pain. In one study, hardware failure was a worrying 36%. Hardware failure can often be treated with additional surgery. This is to remove and replace the damaged hardware.
Hardware becomes loose
Lumbar fusion uses screws to stabilize the spine. Screws can become loosen due to the same forces that can break hardware. This can lead to spinal instability and pain. A total of 1 in 10 patients with a low back fuse will require a second operation to correct non-union or hardware failure.
Additional complications from L5 S1 Lumbar Fusion
Lumbar fusion can lead to a variety of issues. Adjacent Segment Disease (Spinal Muscle Injury) are the two most important.
Adjacent Segment Disease
The disc acts as a shock absorber. Fusion surgery eliminates this shock absorber, placing more stress and forces on the discs above and below the level for the fusion. This extra force can cause injury to the discs and facet joints, leading to arthritis and degeneration. This is a serious problem with a 9 percent chance. This could lead to further surgeries, including fusions.
Spinal Muscle Injury
The spine is supported and stabilized by the spinal muscles. Lumbar fusion can seriously compromise the health and integrity these muscles. This can cause spine instability, degeneration, arthritis, and other injuries. VA was a recent patient who had this problem. VA had lumbar fusion many years ago to relieve severe low back pain. The pain did not improve after the surgery.
The MRI of his low back is shown below. It is the most important for the death of the crucial low back muscles. This is a cross-sectional image of the MRI. The yellow arrows on the right point to healthy dark spine muscles. The left image is from after the surgery. The yellow arrows indicate the injured muscles which are now dead due to fusion surgery.
What is Lumbar discectomy?
Discectomy simply means “cutting out the disc”. A discectomy can take place anywhere along the spine, from the cervical (neck) to the low back and lumbar (lumbar). The surgeon will reach the disc by removing a portion of the lamina and muscles from the posterior (back) side of the spine.
The surgeon removes a portion from the lamina to access the disc. The lamina, which forms the spine’s backside and acts as a roof around the spinal cord, is what the surgeon removes. The spinal nerve is then retracted to the opposite side. Depending on the case, one or more discs (single-level or multi-level) can be removed.
There are many surgical techniques and tools that can be used for discectomy. A “open” procedure uses large incisions and muscle retraction to allow the surgeon to view the disc. A microendoscopic discectomy, or minimally invasive technique, uses a smaller incision.
To tunnel through the muscles, a series of gradually larger tubes called dilators are used. Special instruments allow the surgeon to see and work in a smaller area. Minimally invasive incisions cause less damage to the back muscles, and can reduce recovery time. The best technique for you will be determined by your surgeon.
Patients who work hard, are competitive, or have severe spinal instability may need to have fusion done simultaneously with discectomy. Fusion is a combination of bone graft and hardware (screws/plates), to join two vertebrae. The two vertebrae become one bone during the healing process. A herniated disc in the lumbar spine is not usually required to fuse.
Who are the candidates?
If you have the following:
- Diagnostic tests (MRI, CT and myelograms) that reveal a herniated disc
- You feel severe pain, weakness, or numbness at your foot or leg.
- Leg pain (sciatica), worse than back pain
- Symptoms that do not improve with medication or physical therapy
- Cauda Equina Syndrome is a condition that causes leg weakness, loss in feeling in the genital region, and loss of bladder control or bladder control.
Leg pain may be treated with posterior lumbar discectomy.
- Bulging disc or herniated disc. The gel-like substance within the disc can burst or rupture through the weaker area of the surrounding wall (annulus). This material can cause irritation and swelling by pressing on a nerve. 1).
- Degenerative disc disease: When discs wear out naturally, bone spurs develop and the facet joints become inflamed. The discs shrink and dry out, losing flexibility and cushioning. The disc spaces shrink. This can lead to disc herniation or stenosis.
The surgical decision
After a few months, most herniated discs will heal. While your doctor may suggest treatment options, it is up to you to decide if surgery is right for yourself. Before making a decision, make sure you weigh the benefits and risks. Only 10% of patients with herniated disc problems feel enough pain after six weeks of nonsurgical treatment before they are ready to consider surgery.
Who is responsible for the procedure?
Spine surgery can be performed by either an orthopedic or neurosurgeon. Many spine surgeons are trained in complex spine surgery. Ask your surgeon for details about their training, especially in complex cases or if you have had multiple spinal surgeries.
What happens before and after surgery?
You will need to sign consent forms and other forms in order for the surgeon to know your medical history (allergies/vitamins/bleeding history, anesthesia reactions, prior surgeries, etc.). Talk to your doctor about all prescription, over-the counter, and herbal supplement medications. A few days prior to surgery, you may need to have pre surgical tests such as a blood test, electrocardiogram, or chest X-ray. Talk to your primary care physician before you stop taking any medications.
Keep taking the medication your surgeon has recommended. All non-steroidal anti-inflammatory medications (ibuprofen and naproxen) should be stopped. Blood thinners (Coumadin and aspirin; Plavix, etc.) 7 days prior to surgery. To avoid bleeding and other problems, stop using nicotine and alcohol one week prior to and two weeks after surgery.
Before you have surgery, you may be asked to wash the skin with Hibiclens or Dial soap. It kills bacteria and prevents infections at the surgical site. Avoid getting CHG in the eyes, ears and nose.
Morning of surgery
- If you are told otherwise by the hospital, don’t eat or drink until midnight before your surgery. Allowable medicines may be taken with a small amount of water.
- Use antibacterial soap to wash your skin. Wear loose-fitting, freshly washed clothing.
- Flat-heeled shoes should be paired with closed-backs.
- Remove make-up, hairpins, contacts, body piercings, nail polish, etc.
- All jewelry and valuables should be left at home.
- A list of medications, including dosages and times of use, is helpful.
- A list of your allergies to medications and foods.
- To complete paperwork and perform pre-procedure checks, arrive at the hospital two hours prior to your scheduled surgery. An anesthesiologist will discuss the risks and effects of anesthesia with you.
What happens during surgery?
The procedure consists of five steps. The procedure usually takes between 1 and 2 hours.
Step 1: Prepare the patient
The anesthesia will be administered to you as you lie down on your stomach on the operating table. After you have fallen asleep, roll onto your stomach and support your chest with pillows. You must clean and prepare the area where the incision is to be made.
Step 2: Make an incision
A fluoroscope, a special X Ray device, is used to guide the surgeon through the skin to locate the disc and affected vertebrae. An open discectomy involves a skin incision made along the middle of the back, over the affected vertebrae. The number of discectomy procedures performed will determine the length of the incision. An incision of one level is approximately 1 to 2 inches in length. To expose the bony vertebra, the back muscles must be pulled down on one side. To confirm the correct vertebra, an X-ray is taken.
A 1- to 2-inch incision (black line), is made at the center of your back for an open discectomy. The muscles that are over the vertebrae must be retracted to one end. A small stab entry (greenline) is used to perform a minimally invasive discectomy.
A minimally invasive discectomy involves making a small incision to the back. The next step is to pass progressively larger dilators, one around each other, to slowly separate the muscles and create tunnels to the bony vertebrae. To perform a minimally invasive discectomy the muscles are gradually dilapidated with larger tubular retractors in order to access the bony lamina.
Step 3: Make a laminotomy
The next step is to make a small incision in the lamina above and below the spinal cord using a drill or bone-biting tool. You can perform a laminotomy on either one or both sides (unilateral), or on multiple levels of vertebrae. Laminotomy is a procedure that removes bone from the lamina. To expose the herniated disc, you can gently reflect the nerve root and spinal cord.
Step 4: Remove the disc fragments
After removing the lamina, the surgeon gently retracts its protective sac. To locate the herniated disc, the surgeon uses a surgical microscope. To decompress the spinal root, the surgeon only removes the ruptured disc. The disc is not completely removed. The entire disc is not removed.
The nerve root is freed from the herniated disc material. Fusion is not usually performed for a single-level lumbar discectomy. Fusion may be used to treat other conditions such as spinal instability or recurrent disc herniation.
Step 5: Close the incision
The retractor that holds the muscles together is removed. Stitches or sutures are used to join the muscle and skin incisions. The incisions are closed using skin glue.
What happens after surgery?
In the postoperative recovery area, you will be awake. You will be closely monitored for blood pressure, heart rate and respiration. Any pain will be treated. You can then begin to move, such as sitting in a chair or walking. Most patients are able to go home that day. Others can be discharged from the hospital within 1 to 2 days. For the first 24 hours, ensure that someone is available to assist you at home.
For 2 weeks following surgery, or until your follow up appointment, you should follow the instructions of your surgeon for home care. In general, you can expect:
Restrictions
- Avoid twisting or bending your back.
- Do not lift more than 5 pounds.
- There is no need to engage in strenuous activities such as yard work, housework, or sex.
- Do not drive for the first 2 to 3 days, or while you are taking pain medication or muscle relaxers. You can drive if your pain is under control.
- Don’t drink alcohol. It can thin the blood and increase the risk of bleeding. Don’t mix alcohol and pain medications.
Incision Care
- You can shower the day following surgery if Dermabond skin glue is covering your incision. Every day, gently wash the incision with soap and warm water. Do not rub or pick at glue. Pat dry.
- You can shower two days after your surgery if you have steri-strips, staples, or stitches. Use soap and water to gently wash the area every day. Pat dry.
- Cover the incision with dry gauze if there is any drainage. Call the office if drainage occurs after applying more than one dressing in a single day.
- Do not soak the incisions in a pool or bath.
- Do not apply lotion/ointment to the incision.
- After each shower, dress in clean clothes. Clean sheets are a must for your bed. You can’t allow pets to sleep in your bed until you heal.
- At your follow-up appointment, stitches, steri-strips and staples will be removed.
Medications
- Your surgeon may direct you to take pain medication. As your pain subsides, you can reduce the frequency and amount of pain medication. Don’t use pain medication if you don’t feel the need.
- Constipation can be caused by using narcotics. Get plenty of water and eat lots of high-fiber food. Laxatives and stool softeners can be helpful in moving the bowels. There are many over-the-counter options, including Senokot and Miralax, Dulcolax, Senokot and Dulcolax.
Activity
- To reduce swelling and pain, ice your incision for 15-20 minutes three to four times daily.
- If you’re sleeping, don’t stay in one place for more than an hour. More pain can be caused by stiffness.
- Every 3-4 hours, get up and walk for 5-10 minutes. Gradually increase your ability to walk.
When should you call your doctor?
- Fever exceeding 101.5 degrees (unrelieved with Tylenol).
- Unrelieved nausea or vomiting.
- Incision infection signs
- Itching or rash at the incision (allergy Dermabond skin glue).
- Tenderness and swelling in one leg’s calf.
- A new onset of weakness, tingling or numbness in the arms and legs.
- You may experience dizziness, confusion or extreme sleepiness.
Recovery and Prevention
For 2 weeks following surgery, schedule a follow up appointment with your surgeon. Some people may need physical therapy.
The time taken to heal depends on your overall health and the severity of the underlying condition. The incision may cause pain. You may feel some discomfort at the site of surgery. Keep a positive outlook and do your physical therapy exercises diligently if you are prescribed.
With jobs that aren’t physically demanding, most people can return to work within 2 to 4 weeks. For jobs that require heavy lifting, or heavy machinery, some people may have to wait 8-12 weeks before they can return to work.
It is common for back pain to recur. Prevention is the key to avoiding recurrence.
- Proper lifting techniques
- Proper posture is important when sitting, standing, moving and sleeping.
- Appropriate exercise program
- A well-designed work space
- Healthy weight and lean body mass
- Positive attitude and relaxation techniques (e.g. stress management) are key.
- No smoking
What were the results?
Patients who have had lumbar discectomy are able to achieve good results in between 80 and 90% of cases. The results of a study comparing surgery and nonsurgical treatment for herniated discs were:
- Surgery is more beneficial for people with leg pain (sciatica), than it is for those with back pain.
- Nonsurgical treatment is a good option for people with pain that is less severe or worsening.
- Patients with moderate to severe pain that had surgery experience a greater recovery than those who didn’t.
- Similar to open discectomy, minimally invasive techniques for discectomy have shown comparable results. These newer techniques may have some advantages, such as a shorter recovery time, less blood loss, muscle trauma and a faster operative time. However, they are not suitable for all patients. Ask your surgeon whether minimally invasive microendoscopic discectomy might be right for you.
Nonsurgical treatments may not provide the same pain relief as discectomy. It is not clear if surgery has an effect on what treatment will be required later. Recurrent disc herniations are common in 5-15 percent of patients.
What are the potential risks?
There are always risks involved in surgery. There are many complications to any surgery, including bleeding, infection and reactions to anesthesia. There is a higher chance of complications if spinal fusion is performed simultaneously with a discectomy. A discectomy can lead to the following complications:
Deep vein thrombosis, also known as DVT, is a serious condition that occurs when blood clots develop in the veins of the legs. Lung collapse, or even death can occur if the blood clots travel to the lungs. There are many ways to prevent or treat DVT. So that your blood vessels are moving more efficiently and less likely to clot, get out of bed as soon as possible. You can prevent blood from pooling by using support hose or pulsatile stocks. You may also use drugs such as Coumadin, Heparin or Aspirin.
Lung problems. To heal tissues, the lungs must function at their best after surgery. Mucus and bacteria buildup can cause pneumonia in the affected lungs. The nurse will remind you to take deep, shallow breaths and to cough up often.
Permanent pain or nerve damage. There is a risk that the nerves and spinal cord may be damaged by any spine surgery. Paralysis or numbness can result from nerve damage. The most common reason for persistent pain is nerve damage caused by a disc herniation. Some disc herniations can permanently damage nerves, making them unresponsive to decompressive surgical procedures. These cases may be treated with spinal cord stimulation, or other methods. You should have realistic expectations about the pain you will experience during surgery. Talk to your doctor about your expectations.
Non-surgical Treatments for the L5-S1
The treatment of L5-S1 typically begins with:
- Medication. For pain stemming from L5-S1, you should first try OTC medications (NSAIDs), which are non-steroidal anti-inflammatory drugs (NSI) drugs. Prescription medication such as tramadol and opioids may be prescribed for more severe pain.
- Physical therapy. Physical therapy and exercises can be tailored to address pain originating from L5-S1. These treatments can stabilize the back, keep the muscles and joints healthy for long-term relief and provide a healing environment to the lower back tissues.
- Chiropractic manipulation. Chiropractic adjustment can help to relieve pain from the L5-S1.
- Self-care. You can treat mild to moderate pain at home with heat or ice. Sciatica pain can be treated with heat and ice at home. It is recommended to keep active and do as many daily activities as possible. Although bed rest can temporarily relieve symptoms, it is not likely to provide long-term relief for sciatica.
- A workout routine and quitting smoking can reduce the likelihood of developing problems from L5-S1.
Injection Treatments for L5-S1
After pain relief has been provided by non-surgical options for several weeks, injections might be an option. This is before surgery is even considered.
The following are common injections for L5-S1:
- Lumbar epidural steroid injections. Injecting steroids directly into the spinal epidural area can reduce inflammation and decrease the sensitivity to pain nerve fibers. This will help generate fewer pain signals. These injections are more effective at treating inflammatory pain such as herniated disc fragments or pain due to compression.
- Radiofrequency ablation. Radiofrequency ablation can be used to treat pain originating from the L5–S1 facet joints. To create a heat lesion, a portion of the pain-transmitting nerve is heated using a radiofrequency needle. The resulting lesion stops the nerve from sending out pain signals to the brain.
- For correct needle placement during injections, fluoroscopic (xray) guidance is often used. Fluoroscopic guidance and contrast color help to improve diagnostic accuracy as well as decrease procedural risks.
- Also, injections can be used to diagnose leg pain by using a selective nerve block. This will confirm that the nerve root is the cause.
L5-S1 Surgical Treatments
Surgery may be considered if neurological problems such as weakness and numbness persist despite nonsurgical treatment. When a structural condition is recognized to respond to surgical treatment, surgery may be recommended.
The following surgeries can be performed to relieve the compression of a nerve root or cauda-equina:
Microdiscectomy: This is a procedure that removes a small portion of the disc material close to the nerve root. To relieve the compression, a portion of bone may be removed adjacent to the nerve root.
- Laminectomy: To make more space for the cauda, equina, a portion or all of the lamina (the bone area at the back of the vertebrae) is cut off.
- Foraminotomy is the procedure of enlarging the opening for the spinal nerve root (intervertebral foramen). This relieves compression.
- Facetectomy: To relieve nerve root compression, the facet joints can be trimmed.
- Lumbar interbody Fusion: The degenerated disc in the Lumbar is removed. L5 and S1 vertebrae are then fused with implants or bone transplants. The risk of spinal failure in the S1 segment of fusion surgery is higher than that of L5. This is why it is recommended that an interbody support (device holding the vertebrae together)be added to a fusion at L5 and S1.
One procedure may be performed by a surgeon more than once. A laminoforaminotomy, for example, is when a laminectomy is performed along with a foraminotomy. These surgeries are performed using minimally invasive techniques, but open surgery may be possible in certain cases.
Nonsurgical care may not be appropriate for some patients with progressive neurological problems. Patients may not be suitable for surgery if they have other medical issues or are addicted to drugs. There is a small chance of serious complications such as infection, nerve injury or excessive bleeding. It is important to discuss with your surgeon the risks and other options before you decide to undergo surgery. You should also understand what the consequences could be if you have surgery not performed.
In conclusion
L5/S1 fusion is a major procedure that involves the removal of the L5/S1 disc and stabilization of the L5/S1 spinal bones by hardware. L5 S1 Fusion is indicated for debilitating pain and dysfunction due to degenerative disc disease, slipped disc, fractures, sciatica and scoliosis. Depending on the parameters, success rates can vary.
Patient satisfaction is low. Failure to fuse due to non-union, hardware breaking and hardware becoming loose are all possible complications. Additional complications of fusion surgery include injury to the spinal muscles and adjacent segment disease. Avoiding fusion surgery can avoid these complications.