The most common levels of a herniated disc are L4-5 or L5-S1. The symptoms are characterized by sharp, burning, stabbing pain radiating down the leg from below the knee to the posterior or lateral side. The pain is usually superficial and localized and often associated with numbness and tingling.
Motor deficits, decreased reflexes, and weakness can occur in more severe cases. The most common central disc herniation causes low back pain and saddle discomfort in the S1 or S2 distributions. The nerve roots of the cauda Equina may be compressed by a central herniated disc, which can cause difficult urination, incontinence or impotence. A medical history and physical exam may reveal bowel or bladder dysfunction. To prevent permanent impairment, it is important to immediately refer to a specialist.
The most difficult part of diagnosing patients suffering from a central herniated disc is often the distinction between low back strain or herniated. Low back strain can cause pain that is more severe when the patient is standing or twisting, while central disc herniation can make it worse when the patient is sitting.
This is because of increased pressure on the annular fibers. It may be useful to ask the patient if their pain got worse while they were driving to the appointment or waiting in the waiting area. Sitting and bent postures increase pressure on the intervertebral disc, whereas standing or recumbent positions decrease it7. This is why herniated disc symptoms are worsened when the patient sits.
Anatomy and Structure of the L5-S1 Spinal Motion Section
These structures are common to this motion segment:
L5 and S1 vertebrae. There are many differences between the L5 and S1 vertebrae.
- L5 is composed of a vertebral head in the front and an arch at the back. It has three bony protrusions, a prominent spinous process in its middle and two transverse processes along the sides. These protrusions are used as attachment points for ligaments.
- The sacral base is also known as S1, or the upper and wider ends of the triangular-shaped Sacrum. The body of S1 is composed of the alae, a top-most portion with wings-shaped bones on each side. The median ridge, a bony prominence at the back of the S1 vertebra, is located at the bottom. On the left and right sides of this ridge, there are bony openings called foramina.
- The lumbosacral facet joint lined with articular cartilage join L5 and S1.
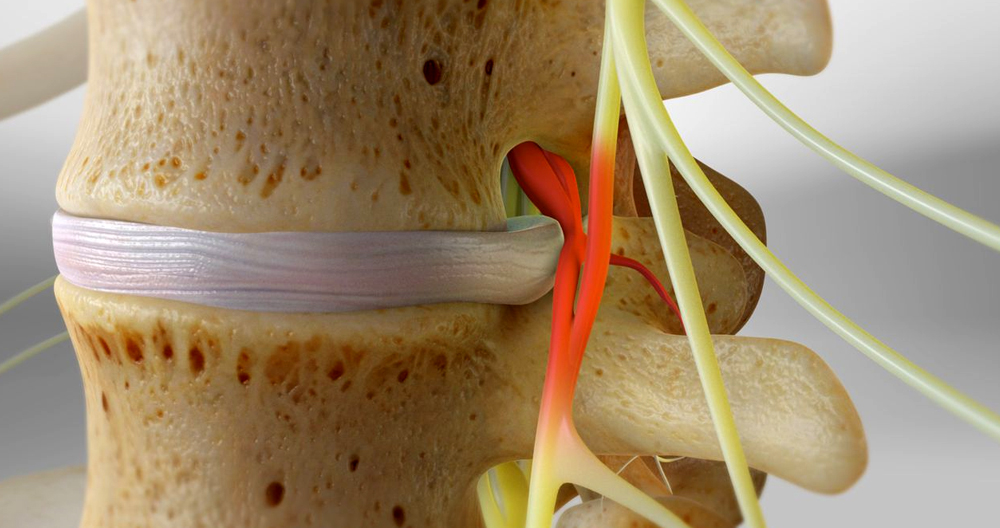
- L5-S1 intervertebral disc. Between the vertebral bodies L5 and S1, a disc is made from a gel-like material (nucleus pilosus), and is surrounded by an thick fibrous ring (“annulus fibrosus”). This disc protects the vertebrae from shock-absorbing and cushioning effects during spinal movements.
- L5 spinal nerve. The L5 spinal nerve roots leave the spinal cord via small bony openings (intervertebral foramina), on the right and left sides of the spinal canal. These nerve roots combine with other nerves to form larger nerves that travel down the spine and down each leg.
- The L5 dermatome, which is a part of the foot, knee, and leg, receives sensations from the L5 spinal neuron, is an area of skin.
- An L5 myotome refers to a group or muscles that are controlled by the L5 spine nerve. It includes specific muscles in the legs and pelvis, which are responsible for foot and leg movements.
- The L5-S1 motion section provides a bony enclosure to the cauda, which are nerves that run down from the spinal cord and other delicate structures.
Common signs of a herniated disc L5/S1
- Back pain: This is the most common sign of a herniated disc L5/S1. Although it may be surprising, most people experience back pain after a herniated disc. It is possible to have a herniated disc and not feel any back pain. This shocked me at first. A herniated L5/S1 disc will cause a sharp, aching pain in the lower back. It can feel tender and akin to spasm.
- Sciatica: The most common cause is a herniated L5/S1 disc. Sciatica refers to the sensation of pain running down the back of your leg. It can be very severe and shooting. My clients describe it as “being stabbed with a hot poker”.
- Pins and needles/Numbness: Sensory changes can occur in the foot and leg due to a herniated disc L5/S1. The funny sensations are usually felt in the feet and toes. For some, it can even be more severe than the pain. The herniated disc presses against the nerve in the spine, preventing it from performing its task correctly. The sensation doesn’t feel normal because some signals aren’t getting through correctly.
- Weakness in the Legs: This symptom can be very alarming. You should see your doctor immediately if you experience weakness in either one or both of your legs. A herniated disc L5/S1 can cause weakness in the legs, particularly in the calf. This is a sign that you need to get it checked out as soon as possible.
What are the L5 – S1 Pain Symptoms?
A typical L5/S1 pain pattern is common for injuries at L5/S1. The severity of the injury will determine whether the L5 or S1 nerve roots are affected. The L5 pain pattern is characterized by pain that runs down the OUTSIDE OF the leg to the outer side of the shin, and then to the outside of the foot. The pain pattern of S1 is similar to “classic sciatica”, with the pain running down the back and sometimes into the toes. These are the most frequent L5-S1 symptoms of pain.
The most common symptoms of a herniated disc L5/S1 are:
- Leg shaking/spasms: These spasms are often confused with sciatica. They cause muscle tension and spasms. This symptom can be treated with a short course in muscle relaxants.
- Troubles with the Bladder or Bowel: This is a serious symptom that must be addressed as soon as possible by a doctor. The herniated disc at the L5/S1 causes the nerves that allow the bladder to function properly and the bowel to stop working. Incontinence can be described as inability to “go”, or feeling that your bladder/bowel are empty. You should consult your doctor immediately. You should contact your doctor immediately if you are unable to do so.
- Numbness in the private areas (or “Saddle”): This is another sign that requires immediate attention. This is another sign that the lower nerves have become compressed to the point they are unable to function properly. This could lead to a serious problem if it isn’t addressed quickly. You should go to the emergency department immediately.
Common Signs and Symptoms that Stem from L5-S1
Disc and vertebral pain starting at L5-S1 can be sudden after an injury, or gradual over time. A dull ache or sharp pain in the lower back is common. Discogenic pain can be worsened by sitting for too long, being in one position, repetitive lifting, and bending.
Radiculopathy symptoms and sciatica can be caused by inflammation or compression of the L5 or S1 spinal nerve roots.
- Pain can be described as a shooting, sharp, or searing sensation in the buttocks, thigh and/or feet.
- Numbness in the toes and/or foot
- A weakness in the foot and/or leg muscles, and inability to lift the feet off the ground (foot drop).
Stabbing pains or aches can also be caused by a skin condition. These symptoms usually affect one leg at the time but can sometimes be felt on both.
Cauda Equina syndrome can occur at L5 to S1 because of injury to the cauda-equina nerves which descend from the spine. This is a medical emergency that can cause severe pain, weakness and numbness in the legs, genital area, and/or both legs. You may also experience loss of bladder and bowel control. This condition should be treated immediately to preserve leg function, and to restore bowel or bladder function.
Nonoperative Treatment
Low back pain and radiculopathy can be common causes of disability. However, most patients find relief regardless of treatment. One study15 found that 70% of patients suffering from radicular pain, whether it was L5 or S1, experienced a significant reduction in leg pain within 4 weeks. It is important to treat patients suffering from symptoms of a herniated disc within the first six weeks.
The family physician is often a teacher and offers advice about how to relieve the symptoms of a herniated disc. Low back pain is most often treated with conservative treatment, which includes limited bed rest, exercise and injections in select cases. The physician must determine the best treatment strategy and goals for each patient. The patient should be fully informed about the condition, including its likely natural history and possible treatment options.
Bed rest is a way to reduce both mechanical pain as well as intradiscal pressure while supine. It is not clear how long bed rest should be for herniated disc patients. However, it is recommended that bed rest last between two and seven days. Studies have shown that prolonged bed rest is not associated with better outcomes16. It has been suggested that patients with herniated discs should be allowed to continue their normal activities while recovering.17 This can lead to deconditioning, bone mineral loss and economic loss.
It is not clear if aerobic exercise can be used to relieve radicular pain. Some believe strengthening the abdominal and back muscles can alleviate symptoms, reduce weight, and ease anxiety and depression. Patients and their families can easily learn massage and exercise techniques. After sufficient strength and pain relief have been achieved, extension and isometric exercises should be performed first. Then, flexion exercises can be allowed. Because flexion exercises place the most strain on the intervertebral disc, flexion exercises should be delayed.