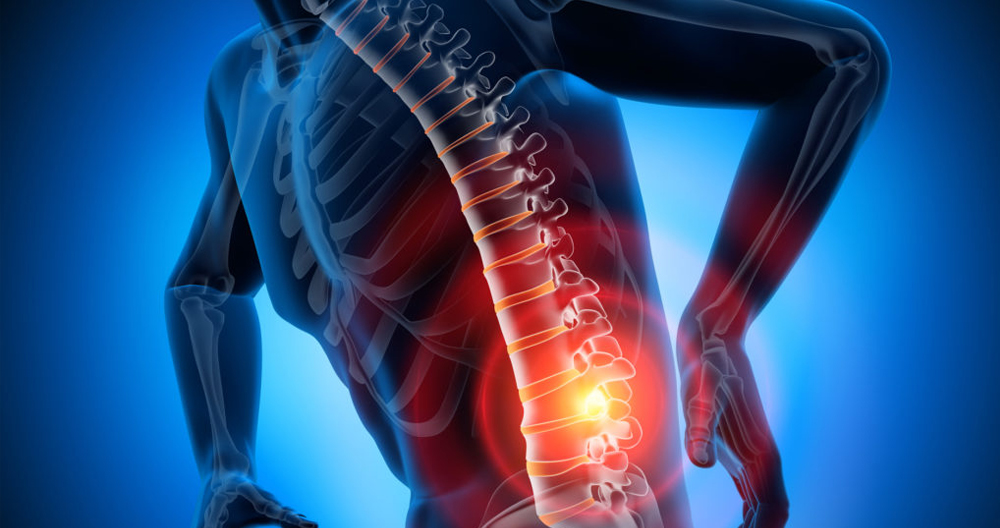
A herniated spinal disc refers to an injury to the backbone or spine. A series of bones (vertebrae), are located in your spine. They run from the base of you skull to your tailbone. Your vertebrae have round cushions called discs between them. The discs act to cushion your bones so you can bend and move comfortably. A herniated or ruptured disc occurs when one of these discs bursts or leaks.
Are Herniated Discs Common?
Each year, approximately 2% of people experience a herniated distal. Herniated dislocated discs are the most common cause of neck, arm, back, leg and/or joint pain (sciatica). While they can occur anywhere along your spine, herniated dislocations most often occur in the neck or lower back. It is rare for herniated disc to occur in the mid back.
Who gets herniated disc?
Most people who have a herniated disc are between the ages 30-49. The problem is more common in men than in women. Other risk factors include:
- Sitting for prolonged periods in the exact same position.
- Being overweight.
- Lifting large objects.
- Repeated twisting, bending, and bending is required for work, hobbies, or sports.
- Smoking.
During the physical exam your doctor will check your back to see if there is any tenderness. For the purpose of diagnosing the root cause of your pain, you might be asked to lie flat or move your legs to different positions.
Your doctor may also conduct a neuro exam to determine if you:
- Reflexes
- Muscle strength
- Walking ability
- Ability to feel vibrations, pinpricks, and light touches
A physical exam and medical history are enough to determine if a herniated or bulging disc is present. If your doctor suspects you may have another condition or is interested in determining the extent of nerve damage, he/she might order any or all of these tests.
Imaging tests
- X-rays. Plain Xrays are not able to detect herniated spinal discs. However, they can rule any other causes of backache such as an infection or tumor.
- CT scan. CT scanner creates cross-sectional images by combining Xrays from various directions.
- MRI. Radio waves and strong magnetic fields are used for images of the internal structures. This test can help to identify the exact location of the herniated nerve and determine the affected nerves.
- Myelogram. Before a CT scan is done, a dye will be injected into the spinal fluid. This test can reveal pressure on the spinal cord, nerves, and other conditions such as multiple herniated or damaged discs.
Nerve testing
Nerve conduction studies and electromyography measure the movement of electrical impulses along nerve tissue. This can be used to pinpoint the exact location of nerve damage.
- Nerve conduction research. Through electrodes placed on the body, this test measures electrical nerve impulses. This study measures nerve impulses when a small amount of current passes through the nerve.
- Electromyography is also known as electromyography. An EMG involves a doctor inserting a needle electrode under the skin into various muscle groups. The test determines whether muscles are active or contract during the test.
How do I avoid a herniated disc?
It is impossible to prevent a herniated disc from happening. There are ways to reduce your risk.
- Proper lifting techniques should be used. Avoid bending at the waist. While bending your knees, keep your back straight. You can support the load with your strong legs.
- It is important to maintain a healthy weight. Excessive weight puts pressure upon the lower back.
- Practice good posture. Learn how to improve the way you walk, stand, sit and sleep. Good posture reduces strain on your spine.
- Stretching. You should take breaks from sitting for prolonged periods.
- Avoid high-heeled heels. This shoe can throw your spine out alignment.
- Exercising regularly. Workouts that strengthen your back or abdomen muscles will support your spine.
- Stopping smoking. Smoking can make your discs more fragile and prone to bursting. Consider quitting smoking.
What is the outlook of people with herniated discs?
For as high as 90% of people, herniated disc pain will resolve on its own. You should feel better within one month. If you are still not feeling better, you should consult your healthcare provider. Some people require more extreme medical measures such as spinal injections and surgery.
Can a herniated disc get worse?
If left untreated, a herniated distal disc can worsen. If you continue to do the same things that caused it, for example, your work, this can make it worse. A ruptured disc that is worsened can lead to chronic pain and loss control. If symptoms persist even after receiving conservative care for four to six months, you should consult your healthcare provider.