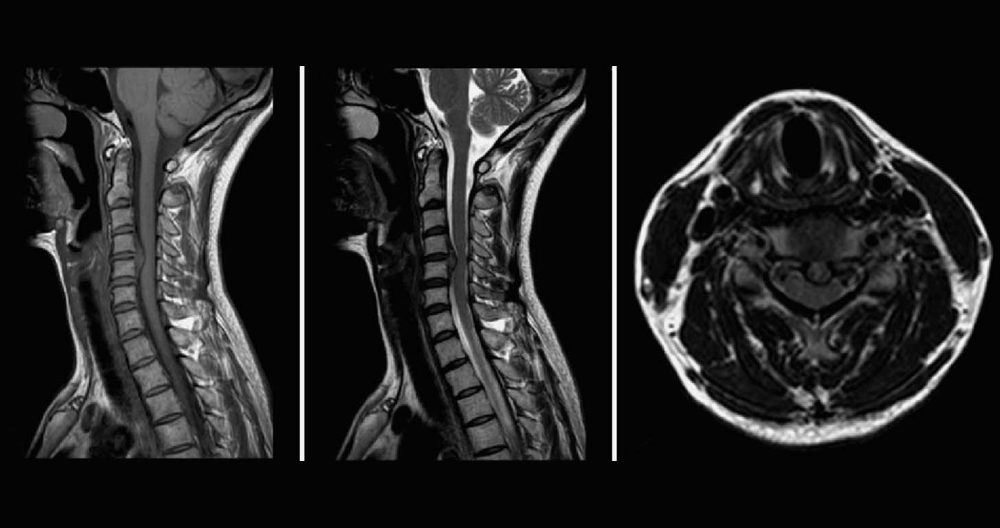
Stress testing of the cervical spine reveals increased pressure to the spine when it is in an upright position. It also includes flexion and extension views (looking upward and downward). When a patient lies down during traditional supine MRI, the stress on the discs is minimal. It may show a slight disc bulge or nothing at all. The disc material is compressed when the table is tilted vertically. This causes the disc material to protrude or herniate, pinching the spinal cord, and causing pain.
In flexion, you look downwards to increase pressure on the disc. This can cause spinal cord compression and herniation growth. Many patients report feeling more pain or numbness at the fingertips. Supine images often fail to show disc herniation and spinal cord compression. MRIs taken in weight bearing or flexion/extension reveal the source of the patient’s pain.
The Stress Test MRI is used to help doctors understand and diagnose positional symptoms. Although patients may feel relief when they lie down, pain, numbness and weakness often increase when the patient is in an upright or weight-bearing posture.
Diagnostic, weight bearing images can show pinched nerves and injured discs. These images may be able to explain the patient’s symptoms in a way that is not possible with traditional supine imaging. Traditional supine MRIs may miss up to 30% of spinal injuries. Ask for a Stress Test MRI if you feel more pain or numbness while standing or sitting. This is your MRI – do not lie down.
Overview
A herniated disc is when the gel-like core of a spinal disc bursts through the tough outer wall. This is similar to how jelly doughnut fillings are squeezed out. When the disc material touches or presses on a spinal nerve, it can cause pain in the neck or arms as well as tingling and numbness. The first steps to recovery include rest, pain medication and spinal injections. Most people feel better within six weeks. They can then return to their normal activities. Surgery may be necessary if symptoms persist.
Anatomy of the Discs
The spine is composed of 24 bones, called vertebrae. The cervical (neck) portion of your spine supports your head weight (approximately 10 lbs) and allows for you to flex your head from side to side and 180 degrees. The cervical vertebrae are numbered from C1 through C7. The discs are shock absorbers that prevent the vertebrae rubbing together. The annulus is the outer ring of a disc. It is made up of fibrous bands that connect between each vertebra’s bodies. The nucleus, a center of gel-filled material in each disc, is located at the middle of each disc. A pair of spinal nerves branch out from your spine at each level. Your spinal cord and spinal nerves function as a “telephone” that allows messages or impulses to travel back-and-forth between your brain, body, and spinal cord to control sensation and movement.
What is a herniated cervical disc?
When the gel-like core of your disc bursts through the disc’s tough disc wall (annulus), it is called a herniated disc. Your spinal nerves are affected by the gel material, which can cause a chemical irritation. The pressure from the herniated disc causes spinal nerve inflammation and swelling, which can cause pain. The herniation will shrink over time and you might experience some or all of the relief that you are seeking. Most cases of neck or arm pain will resolve within 6 weeks.
Normal disc and herniated disc. The nucleus gel material, which is made up of gel and other substances, escapes from the annulus disc and compresses spinal nerves.
A herniated disc can be described using different terms. A bulging disc (also known as protrusion) is when the disc annulus is not damaged but forms an outpouching which can press against nerves. True herniated disc, also known as calming-fluid (or slipped disc), occurs when the disc annulus cracks/ruptures, allowing the gel-filled middle to escape. Sometimes, the herniation can be so severe that a fragment is formed. This means that the disc has been completely removed from the spine.
What are the signs?
The symptoms of a herniated disc can vary depending on where it is located and how you feel about pain. A herniated cervical disc can cause pain radiating down your arm and into your hand. There may be pain near or on your shoulder blades, as well as neck pain when you turn your head or bend your neck. Muscle spasms can occur when muscles tighten and become uncontrollable. Sometimes, the pain can be accompanied by numbness or tingling in your arm. Also, muscle weakness may occur in your handgrip, triceps and biceps.
It is possible that you felt pain the first time you woke up. This could be due to a traumatic event or injury. Some patients find relief by elevating their arm behind their heads, as this relieves pressure on their nerves.
What are the causes of this?
Injuries and improper lifting can cause disc bulging or herniation, or they can happen spontaneously. Aging is an important factor. Your discs become more fragile and dry as you age. The disc’s tough outer fibrous wall may become weaker. A tear in the disc’s outer wall may cause the gel-like nucleus to bulge or burst, causing nerve pain. Early disc degeneration can be caused by genetics, smoking, as well as a variety of occupational or recreational activities.
Who are the affected?
People in their 30s and 40s are most likely to have herniated discs. However, older people and those in middle age are more susceptible to the condition if they engage in strenuous exercise. The neck is home to only 8% of herniated discs.
What is the process of diagnosing a condition?
Consult your family doctor if you feel pain. To understand your symptoms and any previous injuries or conditions, your doctor will conduct a comprehensive medical history. The doctor will also determine if there are any lifestyle issues that may be causing the pain. The doctor will then perform a physical exam to identify the cause of the pain, and check for weakness or numbness.
One or more of these imaging studies may be ordered by your doctor:
Magnetic Resonance Imaging (MRI), a noninvasive scan that uses a magnetic field in combination with radiofrequency waves, gives a detailed view to the soft tissues of the spine. Contrary to X-rays, nerves and discs can be clearly seen. The dye (contrast agent), may be injected into your bloodstream. An MRI will detect the disc that is damaged and any nerve compression. An MRI can detect bone overgrowth, spinal cord tumors or abscesses.
Myelogram, a specialized Xray in which dye is injected through a spinal tap into the spinal canal, is called a myelogram. The images are then recorded by an X-ray fluoroscope. A myelogram is made with a dye that appears white on X-rays. This allows the doctor to see the canal and spinal cord in detail. Myelograms may show pinched nerves due to a herniated disc, bony growth, spinal cord tumors or spinal abscesses. This test may be followed by a CT scan.
The non-invasive CT scan uses an Xray beam and a computer, to create two-dimensional images of the spine. You may be injected with a dye or contrast agent. This test can be used to confirm which disc has been damaged.
EMG (Electromyography) and NCS (Nerve Conduction Studies): EMG (Electromyography) and NCS (Nerve Conduction Studies) measure the electrical activity in your nerves. The results of the electrodes or small needles are placed into your muscles and recorded by a special machine. A herniated disc puts pressure on the nerve root and the nerve can’t supply normal movement and feeling to the muscle. These tests can detect nerve damage or muscle weakness.
X-rays look at the bony vertebrae of your spine. They can show your doctor if they are too close together, arthritic changes or bone spurs. This test cannot diagnose a herniated disc.
Diagnosis of Cervical Radiculopathy Using a Herniated Disc
After reviewing the patient’s medical history and conducting a physical exam, cervical radiculopathy can usually be diagnosed from a herniated disc. To confirm the diagnosis of cervical radiculopathy, the doctor may use one or more provocative diagnostic tests, such as Spurling’s. The test involves the patient being asked to bend or twist their head towards the painful side in order to see if additional pressure can temporarily or permanently trigger the symptoms.
Advanced diagnostics are available if more information is required to confirm the diagnosis. This would most commonly include an MRI scan. It uses a strong magnet that images the cervical spine to show whether a disc has moved onto a nerve root. A CT scan with myelogram, which is dye injected into the spine to view soft tissues, could be used to image the cervical spine if a patient is unable or unwilling to undergo an MRI.
What are the available treatments?
The first step in recovery is conservative nonsurgical treatment. This may include medication and rest, physical therapy, home exercises and hydrotherapy. A majority of arm pain patients with a herniated disc will feel relief within six weeks. They can then return to their normal activities. Your doctor may recommend surgery if you are unable to respond to conservative treatment, or if your symptoms worsen.
Non-surgical treatments
- Self-care: Most cases of a herniated disc will resolve within two days. Your recovery will be made easier by limiting your activities, using heat therapy and taking over-the-counter medications.
- Medication: Your doctor might prescribe medication, including nonsteroidal anti-inflammatory drugs (NSAIDs), pain relievers, and steroids. For muscle spasms, muscle relaxers may be prescribed.
- Aspirin, naproxen, Alleve, Naprosyn, ibuprofen, Motrin, Nuprin and Advil, as well as celecoxib (Celebrex) are nonsteroidal antiinflammatory drugs (NSAIDs). These drugs reduce inflammation and pain.
- Acetaminophen (Tylenol) can be used to relieve pain, but they don’t have as many anti-inflammatory properties as NSAIDs. Analgesics and NSAIDs can cause stomach ulcers, as well as problems with the kidneys and liver.
- To control spasms, muscle relaxants such as methocarbamol or Robaxin, carisoprodol(Soma), and cyclobenzaprine/Flexeril may be prescribed.
- To reduce nerve inflammation and swelling, steroids may be prescribed. They can be taken orally (a Medrol dose packet) in a tapering dose over a 5-day period. It provides pain relief almost immediately within 24 hours.
- Steroid injections: This procedure is performed under x-ray fluoroscopy. It involves injecting steroids and a numbing drug into the epidural area of the spine. To reduce nerve swelling and inflammation, the medicine is administered directly to the area. Although epidural injections can provide temporary relief for approximately 50% of patients, the effects are usually temporary. To achieve full effects, repeat injections may be necessary. The duration of pain relief can vary, and may last for weeks or even years. Injections can be used in conjunction with physical therapy or home exercise programs.
- Physical therapy: This therapy helps you get back to your full activity and prevents injury. Physical therapists will help you with proper posture, lifting and walking, as well as strengthening and stretching your neck, shoulder and arm muscles. You’ll be encouraged to stretch your spine and increase flexibility by them. Strengthening and exercise are important elements of your treatment. They should be a part of your daily fitness.
- Holistic therapies: Acupressure, yoga and nutrition / diet modifications, meditation, biofeedback, and acupuncture are all useful for managing pain and improving overall health.
Surgical treatments
Surgery may be considered if symptoms persist or are not resolved with conservative treatment. Planning surgery takes into account factors such as age, duration of the problem, medical history, past neck surgeries, and the expected outcome.
Anterior (front of neck) is the most common method for cervical disc surgery. If you need decompression due to other conditions, such as stenosis, a posteriori (from your back) approach might be possible.
- Anterior cervical discectomy and fusion (ACDF): A small incision is made in the neck. To expose the bony disc and vertebrae, the neck muscles, vessels, and nerves are removed. The nerve-pressing portion of the ruptured disc is removed. The herniated material can be removed and the disc space can be filled with bone grafts or cages to form a fusion. Fusion refers to the joining of two or more bones. The graft will eventually fuse to the vertebrae above and below, forming one solid piece. To provide stability and possibly improve the fusion rate, metal plates and screws can be used.
- Anterior discectomy: A moveable device mimicking a disc’s natural movement is inserted into the injured joint space. Fusion eliminates motion while an artificial disc preserves it. They are made of metal and plastic and look similar to knee and hip joint implants. The outcomes for artificial disc are similar to ACDF (the gold-standard), but cervical disc replacement preserves motion, and may avoid adjacent level disease. However, this hypothesis is still a possibility and has not been proven.
- Microendoscopic discectomy is minimally invasive. The surgeon makes a small incision at the back of your neck. To enlarge the tunnel from the vertebra, small tubes called dilators are used. To expose the nerve root or disc, a portion of the bone must be removed. To remove the disc, the surgeon can use either an endoscope (or a microscope). This method causes less muscle damage than traditional discectomy.
- Posterior cervical discectomy: A surgeon makes a small incision at the back of your neck. The spinal muscles are removed to reach the damaged disc. To reach the nerve root, and the disc space, a section of the bony ar is removed. It is important to remove the portion of the damaged disc that is compressing a spinal nerve. To prevent further pinching, the spaces where the nerve roots exit from the spine are often enlarged.
Clinical trials
Clinical trials are research studies that test new therapies, such as diagnostics and procedures, on people to determine if they work and if they are safe. To improve medical care, research is ongoing. You can find information about current clinical trials on the Internet, including details such as eligibility, protocol and locations. The National Institutes of Health, private industry, and pharmaceutical companies can sponsor studies.
Recovery and Prevention
8 out of 10 people experience back pain at some point in their lives. Usually, it resolves in 6 weeks. Regular activity, a positive mental attitude and prompt return to work are important aspects of recovery. It is best for patients to be able to return to a modified or limited duty if your normal job is not possible. You can get prescriptions from your physician for this activity for a limited time.
Prevention is the key to avoiding recurrence.
- Proper lifting techniques
- Proper posture is important when sitting, standing, moving and sleeping.
- A good exercise program is needed to strengthen the abdominal muscles and prevent injury.
- A well-designed work space
- Healthy weight and lean body mass
- Positive attitude and stress management
- No smoking